Medical Billing Services
We help you reduce denials and speed up payments. Enhance your revenue with Reliable and Excellent Medical Billing Services available across the USA. Our goal is to simplify your billing process, so you can focus on your Medical Practice, while we handle all your Medical Billing needs.




Why Choose Us!
Medical Billing Services With UMBS
UMBS is a leading Medical Billing Company offering top-quality services to clients worldwide. We provide a full range of Medical Billing Services, ensuring that all services you offer are correctly coded, and payments are processed quickly.
We support Medical Practices of all sizes by solving issues like delayed, underpaid, or lost claims. Our 24/7 Medical Billing Services provide the help your practice needs to boost revenue.
- Increase cash flow by speeding up claim payments
- Resolve billing issues to prevent payment delays
- Stop revenue loss by fixing billing errors
- Ensure compliance with all medical billing rules
- Get paid faster by reducing claim processing time
- Save costs on hiring and training billing staff
- Reduce paperwork with automated claim processing

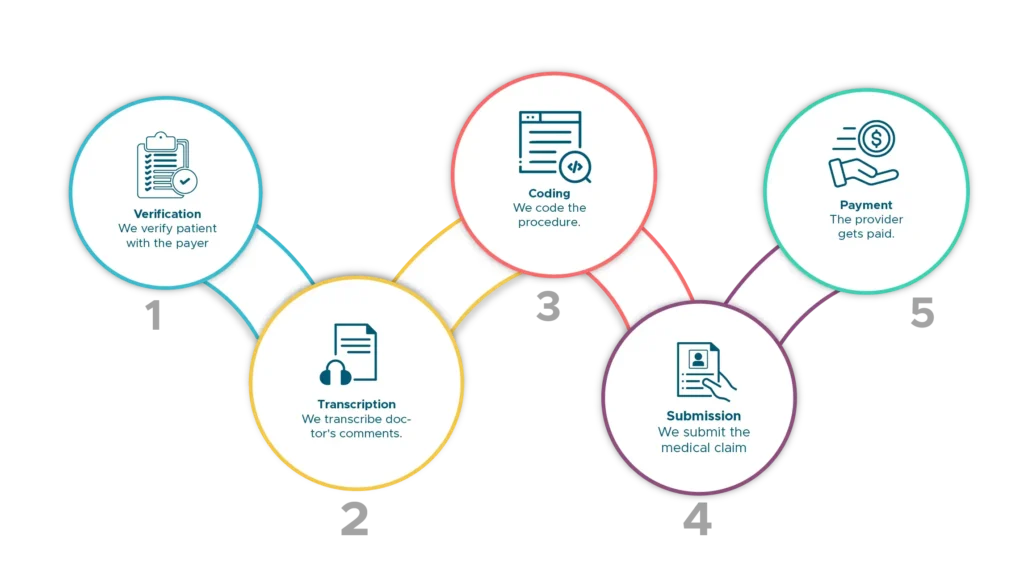
How Our Billing Process WorkWork?
TOP FEATURES
Benefits Of Our Medical Billing Service
KPI Dashboard
Get insight into essential metrics like collected copays and accounts receivable by payer.
Revenue Monitoring
Monitor your practice’s revenue by tracking patient and insurance payments, identifying trends, and measuring financial progress.
Patient Balancing
Send reminder notices to patients with overdue payments and collect outstanding balances to reduce owed money.
Automated Validation
The system checks a patient’s insurance benefits at check-in to avoid billing surprises. Patients are prompted to pay co-pays at this time.
Performance Metrics
Get a quick overview of your practice’s financial performance and create performance initiatives to improve your practice at scale.
Bills Collection
Get a summary of your medical bills, including status (paid, denied, in process, rejected). Our experts will follow up on these bills for you and provide one-click support for any billing problems.
AI Workflow
An AI-powered billing rules engine automatically detects & corrects errors in medical claims, ensuring faster payments and higher reimbursement rates.
Intelligent Billing
Smart billing with a well-defined charge coding means accurate and compliant superbills with zero chances of up/down coding.
Compliance Driven
AI-charged algorithms recommend the appropriate E&M level, and identify and prevent medical fraud abuse to eliminate the need for a separate coder.
Optometrists, Audiologists
Credentialing expands optometrists' and audiologists' reach, delivering essential eye and ear care services to diverse clientele.
Behavioral Health Providers
Our credentialing service helps behavioral health providers join insurance networks, extending vital mental health services to those in need.
"We Provide Resilient
Services"
Outsource to Us Now
Features
With UMBS’s Medical Billing Services, missed payments become a thing of the past. Our service provides clear insights into your performance, helping you collect payments faster and with less work.
Billing Sophistication
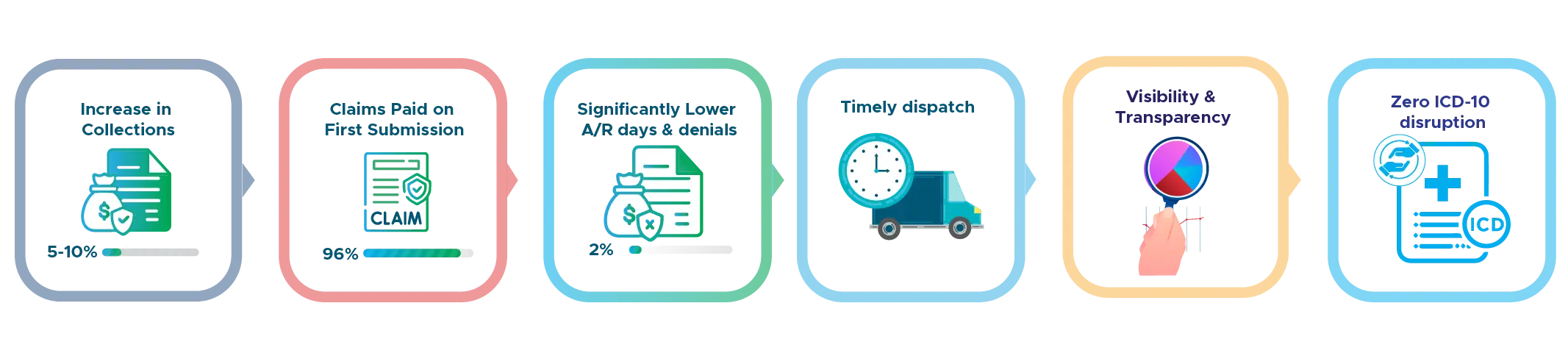
At UMBS, we help you stop revenue loss and increase your collections. We improve your entire billing process, from checking patient eligibility to collecting payments. When you partner with us, you can expect a 5-10% rise in collections within the first few months, and 96% of claims paid on the first try. We also help reduce how long your payments are delayed and make sure patient bills are sent out on time, giving you full transparency into your earnings.

Top Quality Medical Billing Service
UMBS is a leading Medical Billing Company, known for delivering Reliable and Excellent Medical Billing Services to medical offices, clinics, and hospitals. Our services are trusted for being efficient and effective, helping to improve the financial health of medical practices.
Knowledge Base Automation
We constantly update our system to check for billing errors before claims are submitted. This allows 96% of claims to be paid on the first submission, ensuring fast collections.
If a claim is denied, our team handles it for you and updates our system to prevent similar issues in the future. This helps you focus on patient care while we take care of your billing.
For all your Medical Billing needs, UMBS offers Reliable and Excellent Medical Billing Services available across the USA. Whether you’re looking for a Medical Billing Company near me or across the country, we are here to help.
- Fee Schedule Reviews and Analysis
- Eligibility Verification
- Electronic and Paper Claims Submission
- Referral and Authorization Alert
- Incoming Patient Calls
- Account Receivables Management
- Secondary Insurance Billing
- Assistance with EDI, ERA, and Provider Enrollment
- Old Account Receivables Recovery
- Charge Entry – All Specialties
- Posting of Insurance and Patient Payments
- Denial Review and Management
- Appeal of all Denied or Low Paid Claims
- Management Reports
- Extensive Insurance Follow Up
- Patient Statement Processing and Mailing

Secure a Dedicated Billing Expert for Your Clinic's Revenue Cycle Management
Medical billing can be fraught with errors, delays, and inefficiencies, impacting your cash flow and bottom line. UMBS’s billing associates streamline your clinic’s billing process, overseeing the entire revenue cycle management (RCM) with the aid of real-time reports and analytics to ensure seamless operations.
Frequently Asked Questions
We offer a full range of Medical Billing Services, including eligibility verification, coding, claims submission, payment posting, denial management, and Accounts Receivable (AR) follow-up. Our Reliable and Excellent Medical Billing Services ensure that your practice gets paid quickly and efficiently.
We focus on accurate coding, thorough claim reviews, and timely submissions to minimize denials. Our team works diligently to resolve any issues causing payment delays, so your Medical Practice receives the reimbursements it deserves. This process ensures you're covered For all Your Medical Billing Needs.
Yes, we strictly follow HIPAA regulations to protect patient data. Our Medical Billing Company ensures that your information stays confidential and secure at all times.
Our efficient processes help speed up payments significantly. We focus on quick claims submission and Accounts Receivable (AR) follow-up to ensure fast reimbursements for your Medical Practice.
Outsourcing your Medical Billing Services to us means reducing administrative burdens, avoiding costly errors, and focusing more on patient care. You’ll enjoy faster payments, improved cash flow, and the assurance of leading Medical Billing Services. Plus, if you're looking for Medical Billing is near me, we serve practices across the USA.


