Fast & Reliable Insurance Eligibility Verification Solutions
UMBS offers Reliable Insurance Eligibility Verification Solutions that prioritize thorough checks to minimize claim denials and ensure prompt payments for your practice.

Trusted by 790+ Physicians

Catering to 40+ Specialties

70+ Certified Medical Billers & Coders

Open 7 days a week, 7am - 7pm

Insurance Eligibility Verification Services
A critical stage in medical billing and coding is verifying insurance eligibility. Insurance Eligibility Verification ensures accurate and timely information about coverage and reimbursement, which is essential for preventing financial losses.
Without proper checks and balances, healthcare organizations risk financial instability. Failure to validate eligibility or secure prior authorization often leads to delayed payments and claim denials, negatively impacting revenue and collections.
Why is insurance verification important? In 2024, many in the healthcare industry are asking this. The answer is simple: accurate Eligibility Verification is crucial for maintaining financial health and avoiding delayed reimbursements.
Verify patient insurance coverage & co-pays upfront
Patient Eligibility Verification Process
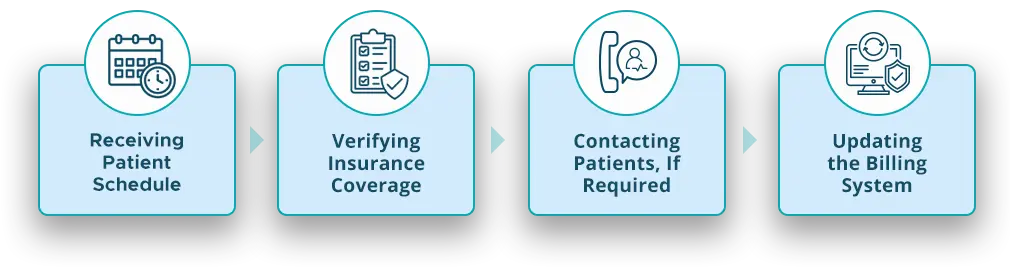
Patient Eligibility Verification With UMBS
Ensuring patient eligibility is key to successful medical billing, helping determine if patients are covered under their healthcare plans.
As a trusted partner, UMBS streamlines Insurance Eligibility Verification Services to save you valuable time. Our services are tailored to practices of all sizes and specialties, ensuring accurate Insurance Eligibility Verification and preventing costly claim denials.
Eligibility and benefits verification helps healthcare providers assess patient coverage before delivering services, minimizing financial risk.

Automated Eligibility Verification — No More Manual Processes!
Our Eligibility Verification Service Covers
Coverage Transparency
We provide clear insights into coverage limits, co-pays, deductibles, and out-of-pocket expenses, both in Dallas, Texas, and across the USA.
Optimized Care Planning
Understanding coverage helps tailor treatment plans to patient benefits, avoiding unexpected costs and ensuring compliance.
Thorough Verification
Our team in Dallas, Texas, verifies insurance eligibility and benefits meticulously, ensuring accurate details across the USA.
Real-Time Insights
Using advanced technology, our verification process offers real-time insights, ensuring the most up-to-date information is always available.
Efficient Claims Processing
With accurate coverage details, our system reduces the risk of claim denials and streamlines billing processes across the USA.
Preventive Measures
Identifying coverage gaps early allows proactive solutions, minimizing claim denials and delays.
Minimized Billing Errors
Accurate verification minimizes errors in claim submissions, improving efficiency and cash flow.
Customized Solutions
We align our verification processes with your practice’s workflows, integrating seamlessly with existing management systems.
Thorough Verification
Our team, based in Dallas, Texas, meticulously verifies patients’ insurance eligibility and benefits, ensuring accurate and up-to-date coverage details all over the USA.

Real-Time Insurance Eligibility Verification
Boost your revenue cycle by partnering with UMBS for real-time eligibility checks. Identifying patient insurance details ahead of time helps prevent claim denials and ensures an error-free billing process, reducing revenue losses and avoiding delays.
Benefits of Outsourcing Your RCM Billing
By outsourcing your RCM billing to United Medical Billing Solutions, you can enjoy the following benefits:
- Cost Efficiency: Lower operational costs by relying on certified professionals.
- Revenue Enhancement: Increase revenue by 20-30% through our proven strategies.
- Transparent Pricing: Pay only for results—no hidden fees.
- Dedicated Support: Personalized service with account managers and support staff.
- Comprehensive Billing: Beyond primary insurance, we handle secondary and tertiary billing for maximum reimbursement.
How to
Manage Claims with Patient Eligibility Verification
Ensuring patient eligibility is a pivotal element of effective revenue cycle management. Proactive insurance claim management is equally crucial. Health insurance verification not only saves time but also minimizes claim rejections. Identifying the patient’s insurance status before providing services is key to reducing claim denials. Proactive eligibility verification significantly enhances overall collections and mitigates reimbursement delays. Moreover, real-time checks on patients’ insurance eligibility contribute to the optimization of the medical billing process.

Failure to verify insurance eligibility can result in delayed or denied payments, increased costs, and patient dissatisfaction. It also leads to claim denials and collection issues.
Collect patient information, contact the insurance payer, verify benefits, determine patient responsibility, and document all details. Electronic verification tools can expedite this process.
Authorization requirements vary by insurance company. Always check with the payer to determine if a procedure needs prior authorization.
The first step is collecting relevant patient information, including insurance policy details, to verify coverage and benefits.
Some insurance payers offer free online eligibility verification tools. However, always ensure the accuracy of the information obtained.


